Understanding laboratory data is increasingly important for patients, caregivers, and healthcare enterprises that want to make informed decisions about diagnostics, treatment considerations, and procurement planning. Among the many routine laboratory indicators, the white blood cell (WBC) count is one of the most frequently ordered tests.
It offers clinicians a fast, high-value snapshot of a patient’s immune activity and potential underlying issues such as infection, inflammation, or hematologic imbalance. While only a licensed clinician can diagnose or treat medical conditions, anyone can benefit from understanding how to interpret WBC results in a general, educational sense.
This article provides a comprehensive overview of what WBC values represent, how differential counts refine interpretation, and what operational stakeholders such as hospital supply teams, pharmaceutical distributors, and even a ceftriaxone injection wholesaler should know about how WBC trends influence demand forecasting and therapeutic planning.
What the WBC Count Measures
A standard WBC test quantifies the total number of white blood cells circulating in a microliter of blood. Although reference ranges vary slightly by laboratory, adult levels commonly fall between approximately 4,000 and 11,000 cells per microliter. Values outside this range do not inherently confirm a clinical condition. Instead, they signal that the immune system may be responding to internal or external stimuli. A high-level understanding of these ranges helps readers contextualize results:
Leukocytosis (elevated WBC count): Often associated with infection, inflammation, physical stress, certain medications, or bone marrow activity.
Leukopenia (low WBC count): May reflect viral infection, autoimmune processes, nutritional deficiencies, medication effects, or bone marrow suppression.
These interpretations are not diagnostic endpoints. They simply establish a framework for professional evaluation.
Why the Differential Count Matters
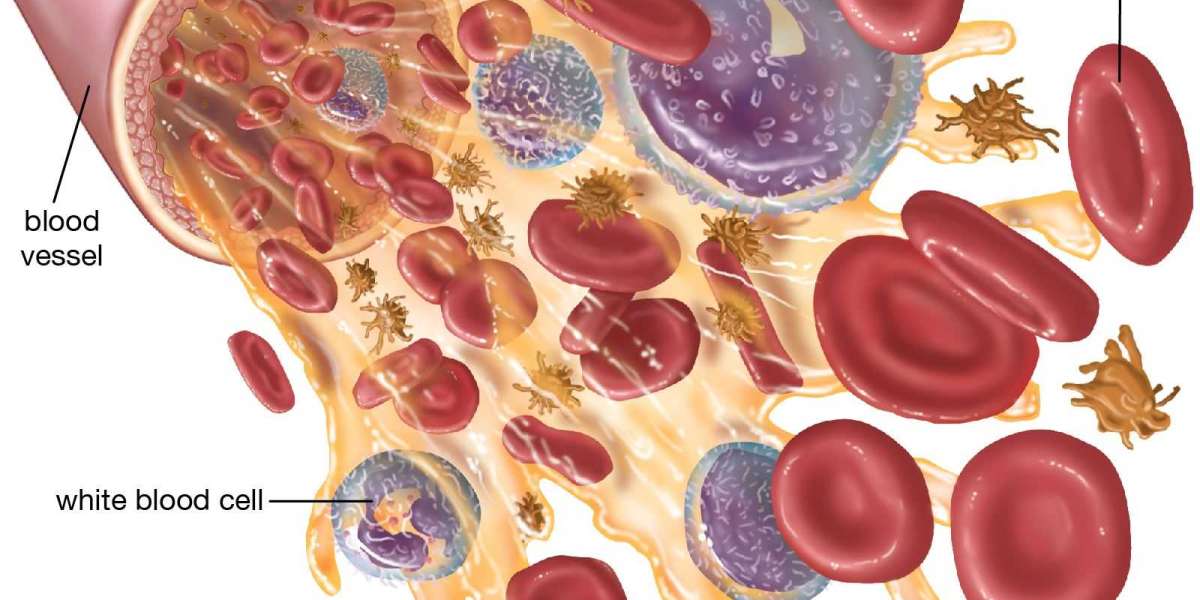
The total WBC count is only one piece of the picture. A WBC differential breaks down the various subtypes of white blood cells neutrophils, lymphocytes, monocytes, eosinophils, and basophils each of which plays a distinct immunologic role. Understanding these categories improves the ability to interpret laboratory data at a strategic level.
Neutrophils
Neutrophils typically constitute 50–70 percent of circulating white blood cells. They respond rapidly to bacterial challenges and inflammatory triggers. A heightened neutrophil count may indicate an acute infection or physiologic stress. From an operational standpoint, this is often the category most closely correlated with antimicrobial utilization trends. When healthcare networks observe sustained regional surges in neutrophilia associated with confirmed bacterial infections, procurement teams may prepare for higher demand for broad-spectrum agents products that a ceftriaxone injection wholesalermay supply, for instance subject to physician judgment and antimicrobial stewardship protocols.
Lymphocytes
Lymphocytes (T cells, B cells, and natural killer cells) are crucial for adaptive immunity. Increased lymphocyte levels may be associated with certain viral conditions or immunologic reactions, whereas lower levels may result from immune suppression or physiological stress. For non-clinicians, lymphocyte trends are useful mainly as contextual indicators rather than diagnostic measures.
Monocytes
Monocytes help manage chronic inflammation and tissue repair. Elevated monocytes may accompany long-term inflammatory states. Although monocyte fluctuations rarely determine procurement decisions, trends in chronic inflammatory diseases may influence long-term forecasting in health systems.
Eosinophils and Basophils
These two subtypes typically appear in small quantities. Elevated eosinophils may be associated with allergic responses or parasitic exposure, while basophils are involved in histamine release and hypersensitivity reactions. These metrics are usually assessed in the context of other laboratory and clinical data.
Putting WBC Results in Context
One of the most important principles when reading WBC results is that context drives interpretation. A single elevated or decreased value is rarely meaningful on its own. Clinicians evaluate:
Patient symptoms
Medical history
Medication exposure
Timing and severity of changes
Other laboratory and imaging findings
Broader epidemiologic patterns
For individuals who are not healthcare professionals, the most practical approach is to treat WBC findings as informational rather than directive. They highlight patterns of immune activity but do not pinpoint specific conditions without professional assessment.
When WBC Changes Influence Organizational Decision-Making
Though WBC results are primarily clinical instruments, their broader patterns carry operational implications across health systems, pharmaceutical distributors, and supply-chain partners. The following areas illustrate how WBC trends can support organizational planning without crossing into clinical decision-making:
1. Demand Forecasting for Anti-infective Medications
Trends in neutrophil-driven infections can correlate with increased orders for antimicrobials. When hospitals report higher volumes of confirmed bacterial pathologies, distributors and wholesalers may adjust inventory management strategies. A stable relationship with a ceftriaxone injection wholesaler becomes particularly relevant when regional infection surges require rapid replenishment of certain antibiotic categories.
2. Capacity Planning in Clinical Settings
Large health systems may track aggregated WBC trends (anonymized and compliant with data privacy standards) as one of several epidemiologic indicators. Significant changes can signal heightened infection prevalence, influencing staffing strategies, bed capacity planning, and triage workflows.
3. Quality and Safety Programs
WBC data can be used to monitor the impact of antimicrobial stewardship initiatives, infection control protocols, and public health interventions. Although these programs primarily focus on clinical outcomes, procurement and logistics teams often coordinate closely with medical leadership to ensure that supply levels align with stewardship objectives.
How to Read Your Own WBC Test Responsibly
Individuals often review test results through patient portals before meeting with their clinicians. Understanding how to process this information constructively can reduce anxiety and enable more effective conversations.
Focus on patterns, not single numbers. One isolated WBC value generally provides limited insight.
Compare values with the lab’s reference range. Ranges depend on the facility; always use the reference printed on the report.
Consider timing and recent events. Physical exertion, stress, and certain medications can affect results.
Prepare questions for your clinician. Use your test results to inform discussion rather than self-diagnose.
Avoid drawing conclusions without professional evaluation. Only a licensed clinician can interpret WBC values in full clinical context.
Conclusion
Reading WBC test results effectively requires understanding what total values mean, how differential counts provide deeper insight, and why context is essential for proper interpretation. While these results are primarily clinical tools, their aggregate patterns can influence health-system operations, pharmaceutical supply chains, and procurement strategies. For distributors and healthcare networks coordinating with a ceftriaxone injection wholesaler, trends in neutrophil-related infections may inform demand planning, provided these activities remain aligned with clinical governance and antimicrobial stewardship.
A clear, structured understanding of WBC data empowers patients to communicate more effectively with clinicians and enables healthcare organizations to make informed, responsible operational decisions.